Learn How Long Suboxone Can Block Opiates
The opioid epidemic has cast a shadow over countless lives. However, Suboxone has emerged as a beacon of hope. It has offered a lifeline to those grappling with opioid addiction. Find out the basics of how Suboxone works and how long it can block the effects of opiates.
What Is Suboxone?
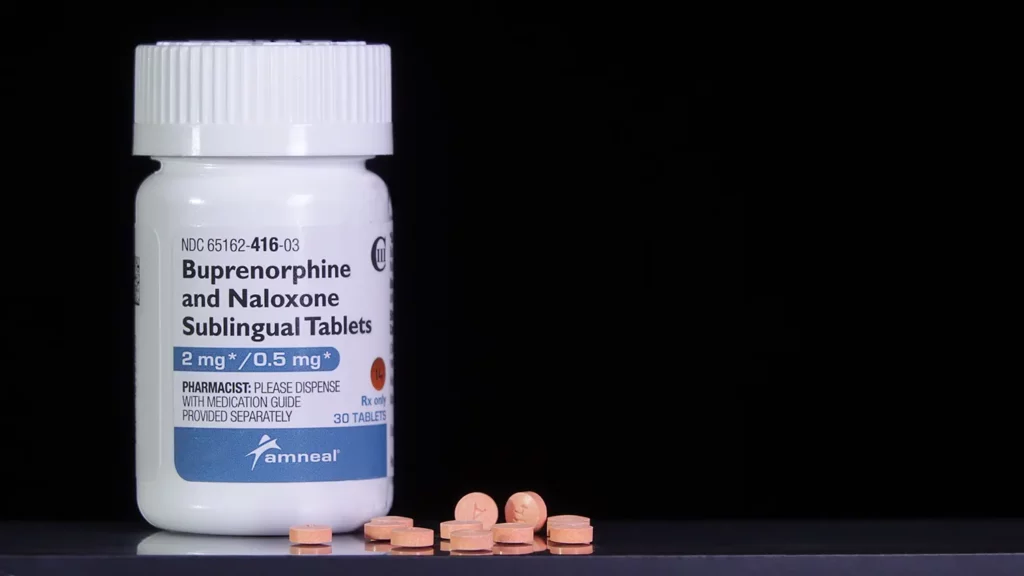
Suboxone is composed of two primary ingredients: buprenorphine and naloxone. Buprenorphine is a partial opioid agonist. This chemical engages with the same receptors in the brain as opiates, but there is a slight difference. Buprenorphine offers partial activation, meaning it provides relief from cravings and withdrawal symptoms associated with opiate dependence. However, it does not provide any feelings of intense euphoria or sedation.
Along with that, Suboxone contains naloxone, a potent opioid antagonist. This component helps to prevent the misuse of Suboxone. When taken as prescribed, naloxone remains dormant. However, should individuals attempt to inject or misuse Suboxone, naloxone activates. In these cases, it induces uncomfortable withdrawal symptoms, discouraging misuse.
Suboxone addresses the challenges individuals face when seeking recovery from opiate addiction. By binding to receptors in the brain, buprenorphine mitigates the physical cravings and withdrawal symptoms that often drive individuals back into addiction. Additionally, naloxone works to deter the misuse of Suboxone, encouraging a safer treatment environment.
Suboxone is currently administered in a medical setting. With better accessibility, this drug can be a viable option for individuals seeking recovery from opiate addiction.
How Long Does Suboxone Block Opiates?
Suboxone blocks the effects of full opioids like heroin, fentanyl, and morphine for 24 to 60 hours. The time frame depends on several factors.
After Administration
Suboxone doesn’t waste time to start moving through the body. Within 15 to 30 minutes of administration, individuals often experience a reduction in cravings and withdrawal symptoms. This immediate effect can be a lifeline during the critical early stages of treatment when the cravings for opiates can be overwhelming.
Short-Term Blocking
After a dose, Suboxone continues to block the euphoric effects of opiates for 24 to 48 hours. If an individual were to use opioids during this time, they would not experience the desired high.
Long-Term Blocking
For individuals on Suboxone maintenance therapy, the blocking effect can help them stay clean for longer periods. When taken as prescribed, Suboxone can provide a sustained barrier against the effects of opiates. As a result, it is an effective tool for long-term recovery. This extended blocking effect helps reduce cravings and minimizes the risk of overdoses.
What Factors Can Affect the Duration of Suboxone’s Block?
The duration of Suboxone’s blocking effect is not set in stone and is influenced by various factors:
Individual Variability
Each person’s response to Suboxone can vary. Metabolism, overall health, and genetic factors can influence how long these effects last for a particular individual.
Tolerance and Dependence
Over time, some individuals may develop tolerance to Suboxone’s effects. In those cases, they may need dosage adjustments to maintain the medication’s blocking properties. Additionally, dependence on Suboxone can occur, necessitating a gradual tapering process.
Comparing the Risks and Benefits of Suboxone
With Suboxone’s ability to block the effects of opiates, it can reduce the risk of an overdose. By alleviating cravings and withdrawal symptoms, Suboxone helps individuals focus on their recovery. In turn, that makes it easier to benefit from therapy and make positive life changes.
Many individuals report an improvement in their overall quality of life while on Suboxone. This drug allows them to regain stability and rebuild relationships. Since Suboxone can serve as a protective barrier against relapse, it gives individuals the time and support to develop healthy coping mechanisms and a drug-free lifestyle.
Suboxone is not without its potential risks and side effects. One of the biggest concerns with Suboxone is the risk of developing reliance on the medication. Without a tapering plan, prolonged usage can lead to physical and psychological dependence.
Unfortunately, Suboxone can be misused by individuals who do not have a legitimate medical need for it. Suboxone can also interact with other medications, especially central nervous system depressants. Combined with other medications, it could lead to increased adverse effects or an overdose. While not everyone experiences severe side effects, some may encounter constipation, nausea, insomnia, or anxiety.
While Suboxone has a ceiling effect that reduces the risk of overdose, taking too much or combining it with other respiratory depressants can lead to breathing difficulties. In addition, some individuals may experience allergic reactions to Suboxone. These symptoms could show up as hives or swelling. Any potential reactions should be addressed by medical personnel immediately.
Rarely, Suboxone can cause liver problems, which may result in symptoms like jaundice, dark urine, or abdominal pain. Suboxone may affect individuals differently, potentially leading to mood swings, depression, or anxiety. Anyone taking this medication should monitor all aspects of their health.
Suboxone Addiction Symptoms
While this medication can be a lifesaver for many individuals, others can become addicted. Like most drugs, there are a few addiction signs and symptoms that may be present in those using Suboxone in an unsafe manner.
Suboxone Cravings
An intense craving for Suboxone can be a clear sign of addiction to the medication. This craving can manifest as a relentless preoccupation with obtaining and using it, even when there’s no medical need. Individuals may find themselves focusing on their next dose while neglecting other responsibilities.
Increased Tolerance
Tolerance occurs when an individual’s body becomes used to the presence of Suboxone. That can reduce the medication’s effectiveness at the prescribed dose. To get the same desired effects, some clients may begin taking higher doses of Suboxone.
Using More Than Prescribed
Sometimes, Suboxone misuse involves taking it in larger amounts than prescribed. This behavior enhances the medication’s effects, giving the person a more intense “high.”
Doctor Shopping
Some individuals engage in “doctor shopping” to maintain their habit. In these instances, the person will seek multiple prescriptions from different healthcare providers. They may not disclose they have an existing Suboxone prescription with another provider. This practice allows the person to get an excess supply of the medication.
Withdrawal Symptoms
Attempting to stop or reduce Suboxone use, particularly without the help of a medical professional, may lead to withdrawal symptoms. These can include:
- Nausea
- Vomiting
- Diarrhea
- Muscle aches
- Anxiety
- Restlessness
- Intense cravings for the medication
Experiencing withdrawal can drive people to continue using Suboxone to avoid these uncomfortable symptoms.
Neglecting Responsibilities
Suboxone addiction can lead someone to neglect personal and societal responsibilities. Individuals may prioritize obtaining and using Suboxone over work, family, education, or social obligations. Doing this can lead to strained relationships and financial difficulties.
Continued Use Despite Consequences
Despite facing negative consequences, such as legal issues or relationship breakdowns, some individuals continue to misuse the medication. This compulsion often overrides the recognition of these adverse outcomes.
Loss of Control
Individuals struggling with Suboxone addiction may feel powerless to control their use. They may make repeated, unsuccessful attempts to cut down or quit but return to misuse Suboxone.
Isolation
Misusing Suboxone can lead to social withdrawal and isolation. Individuals may become secretive about their Suboxone use. They may avoid friends and family members questioning or expressing concern about their behavior.
Lack of Interest in Other Activities
Suboxone addiction can diminish interest in previously enjoyed activities or hobbies. As the focus narrows on obtaining and taking the medication, other aspects of life take a back seat.
Mood Changes
Suboxone misuse can cause mood swings, irritability, and heightened anxiety when not using the medication. These emotional fluctuations can be indicators of an underlying addiction.
Suboxone can be a helpful instrument to assist individuals in overcoming opiate addiction. However, it must be used as part of a structured addiction treatment plan and under the guidance of a qualified healthcare provider.
If you observe indications of Suboxone addiction or misuse in yourself or someone you know, seek professional help immediately. Addiction is a treatable condition. With the correct support and interventions, individuals can regain control of their lives and achieve sustainable recovery.
Treating Suboxone Addiction
Suboxone addiction can be challenging to overcome. Here are some key components of treatment for Suboxone addiction:
Medical Assessment and Supervision
The first step in treating Suboxone addiction is a medical assessment by a healthcare provider experienced in addiction medicine. This examination helps determine the extent of addiction and any co-occurring physical or mental health issues. Medical supervision is essential throughout the treatment process to properly manage withdrawal symptoms.
Tapering
A controlled, supervised tapering plan is often recommended. Tapering gradually reduces the dose of Suboxone to minimize withdrawal symptoms and physical dependence while under medical supervision.
Detoxification
For individuals with a severe Suboxone addiction, a medically supervised detoxification process may be necessary. This process reduces Suboxone under medical guidance to achieve a drug-free state. During detox, healthcare providers can manage withdrawal symptoms and provide necessary support.
Behavioral Therapy
For many, behavioral therapy is a cornerstone of addiction treatment. It helps individuals identify and change their thoughts, behaviors, and triggers associated with addiction. Cognitive behavioral therapy (CBT), contingency management, and motivational interviewing are often used to help those dealing with addiction.
Support Groups
Connecting with others in group therapy who have experienced similar challenges can provide a sense of community and reduce feelings of isolation. Twelve-step programs like Narcotics Anonymous (NA) or Smart Recovery are sometimes suggested.
Personalized Counseling
Individual sessions with a therapist or addiction counselor allow people to receive personalized psychotherapy. Often, individuals can learn about their addiction triggers, helping them develop coping strategies and learn relapse prevention techniques.
Medication-Assisted Treatment (MAT)
In some cases, individuals may transition to another medication-assisted treatment option, such as methadone or naltrexone, under the supervision of a healthcare provider. These medications can help manage cravings and reduce the risk of relapse.
Dual Diagnosis Treatment
Many individuals with Suboxone addiction have co-occurring mental health conditions. Dual diagnosis treatment addresses both addiction and any underlying mental health issues to provide comprehensive care.
Lifestyle and Coping Skills
Developing healthy lifestyle habits and coping strategies is essential for long-term recovery. These habits may include stress management, nutrition, exercise, and finding other healthy alternatives to substance use.
Family and Social Support
When family members and loved ones are involved in the recovery process, it can be an invaluable element for treatment. Family therapy and education programs can help repair relationships and provide a support network.
Aftercare and Relapse Prevention
Once formal treatment is completed, aftercare planning is essential. This step may involve ongoing therapy, support groups, and relapse prevention strategies to maintain sobriety.
Take the Next Step With Charles River Recovery
If you or someone you care about is struggling with addiction, there is hope for recovery. Charles River Recovery assists individuals with substance use disorders, including Suboxone addiction. We offer personalized treatment plans tailored to your specific needs and circumstances. Our approach focuses on addressing the root causes of addiction and equipping you with the tools and strategies necessary for a successful recovery journey.
If you’re ready to take the first step toward recovery or want to learn more about our treatment programs, reach out to the Charles River Recovery team today. Your journey to a healthier, addiction-free life starts here.